The Forgotten Patients
Robert Langreth and Rebecca Ruiz, 09.03.10, 09:00 AM EDT
Forbes Asia Magazine dated September 13, 2010
The mental health industry ignores the 35,000 people a year who commit . A few researchers are trying to change that.
Alexsandra Wixom started experiencing uncontrollable bouts of sadness when she was 15. "I was emotionally off. I cried all the time," recalls the Seattle-area resident, who is now 25. Her mood swings eventually became so wild the former honors student had to quit going to high school. Over the next eight years she saw a psychiatrist every other week. Her doctors tried everything from Zoloft to mood stabilizers to heavy-duty antipsychotics, but none of them helped for long.
By her late teens visions of suicide started floating through her mind. In one nightmare she was a character in a videogame and lay bleeding at the top of a castle and wanted to die. On her 21st birthday in December 2005 the urges became so intense that Wixom checked herself into a hospital for a week. Her second hospitalization came in early 2007, when, while grocery shopping, she was struck with a desire to die. A month later she ended up in the hospital a third time after tripling her daily cocktail of psychiatric drugs in hopes of poisoning herself.
Her behavior might have escalated until it reached a tragic end. But after her last hospitalization Wixom was referred to University of Washington psychologist Marsha Linehan, one of a handful of researchers who specialize in suicidal patients. Linehan diagnosed her with borderline personality disorder, an extreme inability to regulate moods, and prescribed a type of counseling called dialectical behavior therapy.
Wixom spent the next year in group and individual sessions learning practical skills to manage her emotions so that they didn't spiral out of control. They included distress tolerance techniques like plunging her head into ice water, devising ways to distract herself when bad thoughts arose and learning not to leap to the conclusion that one bad day implies a life of misery. She has not been hospitalized since. "DBT is the best thing in the world. It changed my life," says Wixom, who got married halfway through therapy and is raising two daughters, ages 10 months and 2 years. Now with a high school diploma and an associate's degree, she is pursuing a career in online marketing. "Nobody in my boat should be without this."
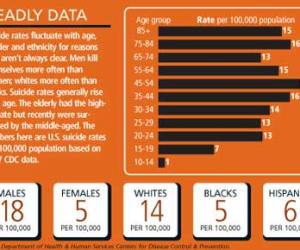
Few suicidal patients get such good treatment. Roughly 35,000 Americans commit suicide each year--more than die from prostate cancer or Parkinson's disease. Another 1.1 million make attempts, while 8 million have suicidal thoughts. Among those aged 15 to 25 it is the third leading cause of death. Yet researchers know astonishingly little about how to treat people who contemplate killing themselves. The subject has been so roundly ignored that the 900-page bible of U.S. psychiatry, the Diagnostic and Statistical Manual of Mental Disorders, offers no advice for doctors on how to assess suicide risk.
Fear, logistics, low research funding and more risk than reward for drug companies all conspire to make suicide the neglected disease. The National Institutes of Health is spending a paltry $40 million in 2010 studying suicide, versus $3.1 billion for research on aids, which kills half the number of Americans. (Another government agency spends $48 million on hotlines and prevention.) Therapists often don't want to treat suicidal patients, and university clinical study review boards are skittish about studying them, says the University of Washington's Linehan.
Big pharma routinely excludes suicidal patients from their tests of antidepressants and other drugs. There's no commercial imperative to crawl out on that limb. Trials in at-risk patients would cost millions of dollars and could take years to perform; they might yield murky results--or worse. A suicide in the drug group could be used by competitors to destroy even a promising drug. The legal overhang is real. GlaxoSmithKline ( GSK - news - people ) has paid $390 million to settle lawsuits related to patients who attempted or completed suicide while on Paxil, Bloomberg News estimates.
As a result, mental health experts have little data on which treatments work in those prone to suicide. In younger patients antidepressants sometimes backfire. Suicidal patients end up in the emergency room, where there is no clear standard besides hospitalization. One unproved method is to make people sign pacts promising not to harm themselves before the next appointment.
"You would think it would be bread and butter for psychiatry," says Harvard Medical School psychiatrist Ross Baldessarini, whose studies have shown that the old drug lithium may be especially effective at quelling suicidal impulses. "But the therapeutic research has been very limited." When he organized a conference on the subject in the 1990s, "nobody had anything to say," he recalls. Columbia University psychologist Barbara Stanley says, "It is one of the most underresearched areas in all of psychiatry."
A handful of researchers are fighting to change this. They argue that it's not enough to throw antidepressants at suicidal patients. Doctors need to treat suicidal thoughts and impulses directly and teach patients coping techniques. They should test drugs specifically for antisuicidal effects and not assume that drugs that help nonsuicidal patients will have the same effects in suicidal ones.
"There is a very smart group of people who think that suicide is simply a symptom of a mental health disorder: Treat the disorder and you will eliminate the symptom," says Catholic University of America psychologist David Jobes, who counsels suicidal patients. "But there is little data to support that. So far the best data we have shows that going after the suicidal [thoughts] and behavior has the biggest impact." Some patients can be depressed for years but not have suicidal thoughts, he says, while others are plagued with suicidal thoughts, yet have only mild depression. Says Vanderbilt University psychiatrist Herbert Meltzer, who has studied schizophrenia patients who are at high risk of suicide: "You need a specifically targeted antisuicide effect."
The research is beginning to show results. Two rigorous trials have demonstrated that therapy that targets the distorted thinking patterns in suicidal patients and teaches coping techniques can reduce the rate of suicide attempts by half. Other studies have shown that something as simple as periodic "caring letters" or checking in on patients, say, once a month can help prevent suicides. Researchers are evaluating safety plans, written documents that patients carry in their pockets to help cope when suicidal urges strike. Studies suggest two drugs--clozapine for schizophrenia and lithium in bipolar disorder--are particularly good at preventing suicide attempts, but both have side effects that limit their use.
The suicide treatment push is gaining support from an unlikely source: the military. It has been stung by suicides in the wake of the Afghanistan and Iraq wars. In 2009 a record 244 soldiers (active and reserves) killed themselves. This year there have been 156 so far. Among other projects the U.S. Army is spending $50 million on an epidemiological study that will search for risk factors that predict which patients are likely to attempt suicide.
Mary Cesare-Murphy, who heads the behavioral health program at the Joint Commission, a nonprofit that accredits hospitals, says health workers are becoming more aware of the role they can play in preventing suicide. In the past "you would hear people saying, 'Well, that's the natural course of the illness,'" she says. Now, she says, workers are much more inclined to believe "interventions can reduce people's drive to kill themselves."
But will early leads in suicide prevention be followed up with breakthrough therapies? It took decades to translate early findings for heart risk factors into lifesaving cholesterol drugs. The logistics of suicide are far more daunting, given the relative rarity of actual suicides among the millions of troubled souls.
Risk factors for suicide are myriad and confusing. As many as 90% of patients who kill themselves are depressed or have other psychiatric problems. The biggest risk factor is a previous attempt. Alcohol abuse, insomnia and anxiety put people at risk, says University of New Mexico psychiatrist Jan Fawcett, who is pushing to get suicide risk assessment into the next DSM edition. External stressors such as joblessness play a role. (U.S. figures on whether suicides increased in the 2008 recession are not in yet, but suicides generally go up in bad economic times.) The very elderly once had the highest suicide rate, but middle-aged men and women in the U.S., 45 to 54 (see graph, below), have surged recently and surpassed them. Why? It's unclear.
Many suicide treatment researchers stumbled into the field. In the 1990s Columbia University's Stanley wanted to offer state-of-the-art treatment to suicidal patients participating in a brain neurochemistry study. "I went into the literature and found nothing--zip," she recalls. "It was a huge shock." When she spoke up about the problem at scientific meetings, she got a frosty reception. Psychiatrists were all too familiar with the state of affairs, she says, but were pessimistic anything could be done. "I was astounded. If you don't study it, how do you ever have hope of making progress?"
The University of Washington's Linehan deserves much of the credit for demonstrating that suicidal patients can be treated. Now 67, she almost became a nun but realized she was too nonconformist. She got into the therapy business in the 1970s after deciding there was too little evidence backing psychiatry. "She started decades ago and has paved the way for others to treat high-risk patients," says psychologist David Rudd, dean of the University of Utah's college of social and behavioral science.
Reading the literature, she realized that many patients suffered something called borderline personality disorder, in which people lack any ability to control everyday emotions. Their feelings spiral out of control at the slightest push, like a car parked on a steep hill without an emergency brake. It has a 10% lifetime suicide rate. "My fundamental theory is that highly suicidal people don't have the skills to regulate their behavior and emotions. ... You have to teach those skills," Linehan says.
She spent years coming up with a combination of techniques to help. Her DBT is a cousin of cognitive behavioral therapy, which focuses on correcting distorted thought patterns that can make people depressed. Her treatment focuses much more on behavioral methods, including Zen acceptance techniques she learned from living one summer in a Buddhist monastery in California and from a Zen master in Germany. DBT teaches patients to tolerate the stresses of the moment, accept that imperfect lives are worth living and gain the skills to cope with raging emotions. The therapy often starts with crisis control. Over the years her group has had a doctor who played Russian roulette with a loaded gun, patients who kicked in walls and one who threatened to kill the President. Some patients come in using so many psychiatric meds they can barely stay awake. Linehan tapers them down to the essential ones. Sometimes she practices tough love. When one patient had her stomach pumped in the er after an attempted antidepressant overdose, Linehan told her parents not to come and had her take a cab home and report for work the next day. "That was the best thing that ever happened to me," says the woman, who recovered, got married and is raising a 2-year-old boy.
Linehan's first small study (1991) showing that DBT reduced suicide attempts was criticized because the patients got intensive treatment by experts like her, which might have accounted for the improvement. But in 2006 Linehan assigned 111 suicidal patients to receive either DBT or intensive treatment using other techniques. Patients on DBT had half the rate of attempted suicides over the next two years and were hospitalized less often for suicidal thoughts, according to the results in the Archives of General Psychiatry.
DBT usually requires six months or a year of twice-weekly sessions, but shorter courses of therapy can also help. University of Pennsylvania researchers found that ten weeks of cognitive behavioral therapy reduced the rate of repeat suicide attempts by half in patients who reported to the emergency room after an attempt. One key was logistics: A huge effort had to be made in tracking the patients and making sure they came to the sessions, says University of Pennsylvania psychologist Gregory Brown.
For frontline docs, Brown and Columbia University's Stanley are testing a safety plan that patients write out with a clinician and keep with them at all times. Essentially a list of distracting things to do and people to call when suicidal urges arise, "it is the equivalent of 'stop, drop, and roll,'" says Stanley. One patient, she says, "went to a bridge, reached into his pocket, realized the safety plan was there--and didn't do it."
Research into how drugs affect suicidal behavior is less advanced. Only one psychiatric drug--Novartis ( NVS - news - people )' clozapine, long used to treat schizophrenia--has been shown to prevent suicide attempts in a large trial, published in 2003, in which it beat Eli Lilly ( LLY - news - people )'s schizophrenia drug Zyprexa by 25%. That result has had little impact on everyday practice because the drug's side effects (especially a rare but life-threatening blood disorder) complicate its use. A Finnish study last year found that clozapine's antisuicide effects outweigh its risk. Numerous factors work against testing psychiatric medicines on suicidal patients, says Novartis Chairman Daniel Vasella. (Vasella, a doctor, insisted on the trial over the objections of some underlings.) So little is known about the biology of suicide that the outcome is unpredictable.
Antidepressants, amazingly, have basically not been tested on suicidal patients. The lack of good data makes it almost impossible to resolve the ancient controversy over whether antidepressants prevent suicide. Eli Lilly, maker of Prozac and Cymbalta, says in an e-mail it would be "neither safe nor ethical" to enter suicidal patients into a trial where they might get a placebo or unproved treatment. GlaxoSmithKline and Pfizer ( PFE - news - people ) also say studies on at-risk patients would be unethical.
Nonsense, says psychiatrist Arif Khan, who runs the Northwest Clinical Research Center in Bellevue, Washington. He has spent years lobbying drug companies to test their psychiatric drugs on suicidal patients but gotten nowhere. "They say it is too risky, we don't know how, we don't have the money--lots of excuses," he says. The real reason, he suspects: drug companies "think that if you exclude patients with suicidal thoughts you will make the drug look better. ... It is cover your ass and hope for the best." The FDA says it supports studies in patients at high risk of suicide and is not holding things up. "We have never stopped any studies from going forward," says Thomas Laughren, director of the psychiatry products division.
One drug that shows promise in suicidal patients is lithium, which has been used for decades to treat bipolar disorder and has been largely displaced by heavily marketed new agents. Bipolar disorder has a very high correlation with suicide; as many as 20% of such patients will kill themselves. Numerous studies by Harvard's Baldessarini and others have gathered medical records of patients on lithium and found an 80% reduction in suicide rates, compared with those taking other drugs. No one is sure why, he says, but lithium may be good at suppressing aggressive and impulsive behaviors.
If the findings hold up, putting more people on lithium could save thousands of lives, especially among those with severe garden-variety depression. But lithium is a tricky drug--small overdoses can be toxic--so doctors are unlikely to change their practice without definitive evidence. Because the drug is not patented, "there is very little commercial interest" in doing a rigorous trial to prove it, says Baldessarini.
Fed up, Khan is spending $2 million of his own to study a combination of lithium and Forest Laboratories ( FRX - news - people )' old antidepressant Celexa in 80 at-risk patients, aiming to show this reduces suicidal thoughts and impulses. Khan has applied for a patent on the combo and formed a company hoping that positive results will convince someone to fund a larger trial. Says he: "I am hoping we can shed some light into this darkness."
www.nmgpsy.com内蒙古心理网